Running a practice
A discussion of medical decision-making for psychiatry billing
Learn how to document MDM to capture clinical complexity, support your E/M code choice, and reduce billing risk in your psychiatry documentation.

January 16, 2026
10 min read
As a psychiatric provider, you have a unique skillset and medical training that allow you to provide comprehensive behavioral health care. These encounters vary in complexity and involve making assessments, interpreting data, and creating treatment plans.
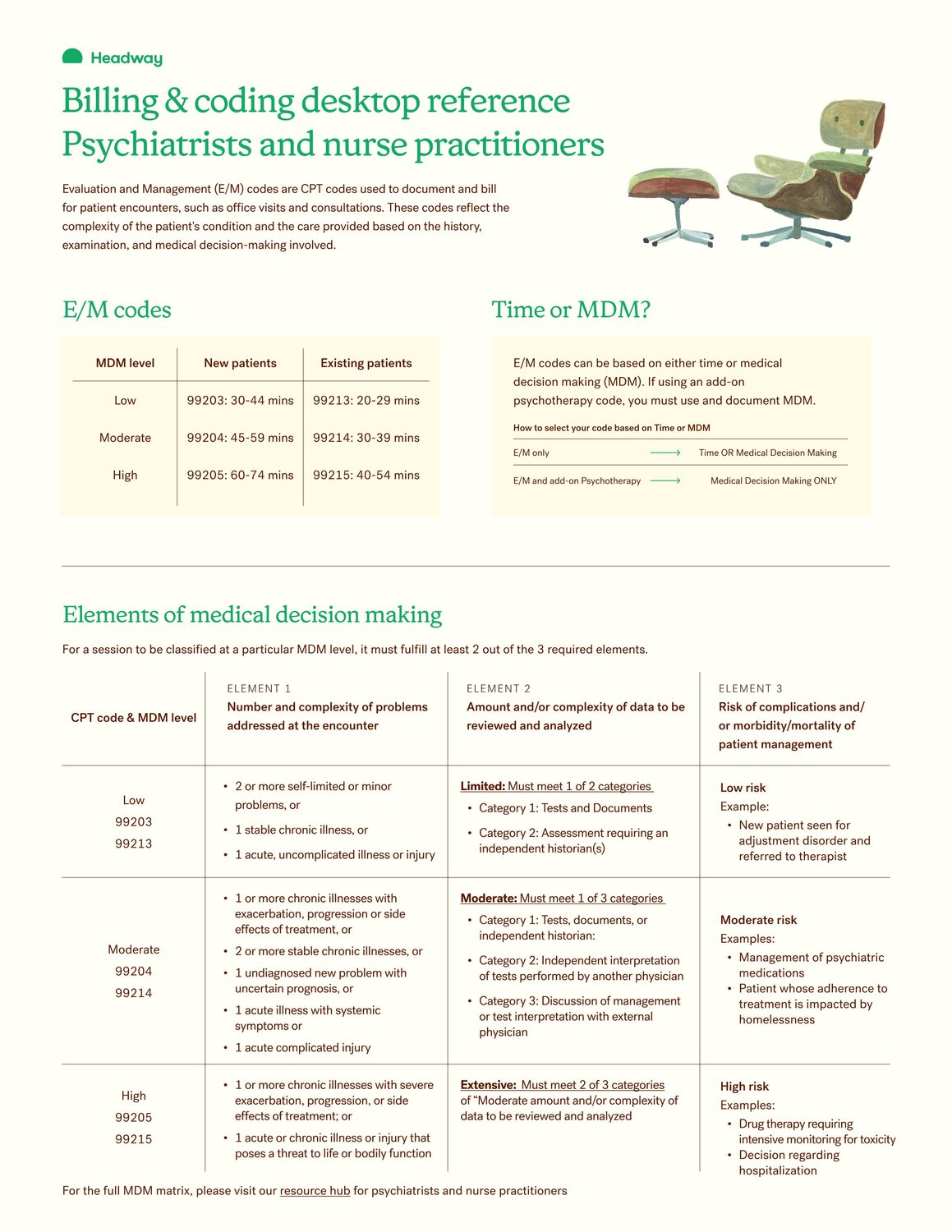
When you’re providing these medically-oriented services, you may choose to bill evaluation and management (E/M) codes. Medical decision-making (MDM) is one of two methods for determining the right E/M code to bill a given patient encounter; the other is time. (However, when billing E/M with add-on psychotherapy on the same date, the E/M level must be selected using MDM, not time.) Thorough and compliant documentation is essential with E/M coding to avoid payment delays and other time-consuming hiccups that can affect your practice.
Below, learn more about medical decision making in psychiatry, and how you can incorporate it into your practice.
Key takeaways
- Medical decision-making is one of two methods used to determine the correct E/M code level for a patient encounter.
- MDM is made up of three core elements and has three main grading levels to help determine the appropriate E/M code and corresponding reimbursement.
- By supporting compliant documentation and billing, Headway makes it easy for psychiatrists and psychiatric care providers to focus on providing effective clinical care.
What is medical decision-making — and what do psychiatrists need to know?
Medical decision-making (MDM) describes the clinical judgment you use to evaluate a patient, interpret relevant information, and determine an appropriate treatment plan. In E/M coding, MDM reflects visit complexity based on:
- the problems addressed
- the data reviewed and analyzed
- the risk of complications and/or management decisions
Evaluation and management (E/M) codes are CPT codes established by the American Medical Association that describe medically oriented services such as assessment, management, care coordination, and clinical decision-making.
You can select an E/M level using either MDM or time. However, the MDM method is required when billing an E/M code with add-on psychotherapy codes, such as 90833, 90836, and 90838. In these cases, the E/M level must be selected using MDM.
Use an E/M code when the visit is focused on evaluation and management of the patient’s psychiatric condition (for example, assessment, medication management, or care coordination). The appropriate E/M code depends on whether the patient is new or established and whether psychotherapy was also provided.
When selecting an E/M level based on MDM, at least two of the three elements (problems, data, and risk) must meet or exceed the requirements for that level: straightforward, low, moderate, or high.
Whether you choose to code for time or MDM, thorough and compliant documentation is essential when you're billing E/M codes. To reimburse providers, payers require detailed backup that illustrates why you provided a certain service based on a patient’s diagnosis and treatment plan.

Practice in-network with confidence
Simplify insurance and save time on your entire workflow — from compliance and billing to credentialing and admin.
The three elements of medical decision-making
According to the AMA, MDM is based on the following three core elements:
MDM element 1: Number and complexity of problems addressed at the encounter
This reflects the conditions you actively evaluate or manage during the visit, and how complex they are. A single, stable condition is lower complexity. Multiple conditions, worsening symptoms, or unstable/severe presentations increase complexity.
MDM element 2: Amount and/or complexity of data to be reviewed and analyzed
This element is evaluated using data categories. The level you meet depends on the mix of data activities completed — such as reviewing records/tests, ordering tests, independently interpreting results, or discussing findings with an external clinician.
MDM element 3: Risk of complications and/or morbidity or mortality of patient management
This represents how risky treatment decisions are (not just how sick the patient is). Starting or adjusting higher-risk medications, managing safety concerns, or making treatment decisions that require close monitoring or carry significant adverse-effect risk generally increases the risk level.
The levels of medical decision-making
For psychiatric providers, E/M codes are graded on three levels of MDM, each with their own criteria for the three elements above.
Low (CPT codes 99203, 99213)
This visit involves a stable or mild condition with limited data and low risk. Medication may be continued without adjustments. For example, a new patient assessed for adjustment disorder and referred to therapy without prescription drug management or safety risk, could be a low-level visit.
Moderate (CPT codes 99204, 99214)
This visit involves managing multiple or worsening conditions, reviewing more complex data, or making treatment changes that carry some amount of risk. For example, medication adjustment for depression with new side effects could be a moderate-level visit.
High (CPT codes 99205, 99215)
This visit involves severe symptoms, significant safety concerns, or high-risk treatment decisions. For example, a patient with suicidality or psychosis starting medications that require intensive monitoring could be a high-level visit.
When the three elements fall into different levels, the overall MDM level is the highest level supported by at least two elements. For example, a patient has a stable chronic condition and you review a limited amount of data (Low problems + Low data). Even if one decision increases risk to Moderate (for example, prescription drug management), the overall MDM level is still Low unless a second element (problems or data) also reaches Moderate.
Medical decision-making chart for psychiatrists
A full table of levels and elements of MDM, reproduced from the AMA, is available below. Click it to view a full downloadable PDF.
Key considerations of medical decision-making for psychiatry
If you’re considering an E/M code for a patient encounter, the following best practices can help ensure your documentation is compliant and effective.
- Document symptom complexity clearly. MDM is often downgraded when psychiatrists under-describe severity of symptoms. Note a patient’s worsening mood, functional impairment, safety concerns, or multiple active diagnoses.
- Capture all the problems you addressed. If you address depression, insomnia, and medication side effects in one patient visit, document each one to reflect the visit’s true complexity.
- Include all relevant data reviewed. Be sure to reference assessment scores, notes from therapists, past medical records, or lab results anytime they inform your treatment.
- Highlight risk associated with treatment decisions. Starting, stopping, or changing medications with major side-effect profiles should be explicitly noted in your documentation.
- Document safety assessments. Suicidal, self-harm, or risk-of-deterioration discussions significantly increase MDM.
- Explain your clinical reason. Briefly note why you chose a specific intervention, dosage, or follow-up plan based on a patient’s diagnosis and treatment plan.
- Avoid vague language. Words like “stable” or “doing fine” without any context may not support higher levels of MDM.
A note on codes requiring medical necessity justification: For each, please ensure that diagnosis codes are documented at the highest level of specificity. Avoid unspecified codes when a more precise option is available.
Medical decision-making’s impact on reimbursement for medication management
Medical decision-making plays an important role in how medication management visits are reimbursed. Accurate MDM supports appropriate E/M levels and ensures psychiatric providers are paid for the true complexity and expertise involved in their work.
When MDM is under-documented, reimbursement often falls short and it creates risk for recoupment and denials. Headway helps close that gap, thanks to coding experts who stay up to date on coding guidelines and insurance company policies. We pair billing support with competitive reimbursement rates and a reliable, transparent bi-weekly pay schedule. With fewer surprises and faster payments, psychiatric providers can focus more on delivering high-quality medication management to the patients who rely on them.
Get admin support for your practice
Medical decision-making is at the heart of psychiatric care, and getting E/M coding right ensures your time, expertise, and clinical judgment are accurately reflected and reimbursed. But navigating documentation, insurance rules, and audits shouldn’t pull focus from patient care. That’s where Headway comes in.
By streamlining insurance workflows, supporting compliant documentation and billing, and reducing administrative burden, Headway helps psychiatrists focus on what matters most: delivering high-quality care with confidence. When your systems work as hard as you do, MDM becomes a tool for sustainability, not stress.
Expand your practice with Headway
Join a network of thousands of mental health providers who have already chosen Headway to streamline their practice and expand their network — at no cost to you.
This content is for general informational and educational purposes only and does not constitute clinical, legal, financial, or professional advice. All decisions should be made at the discretion of the individual or organization, in consultation with qualified clinical, legal, or other appropriate professionals.
© 2025 Therapymatch, Inc. dba Headway. All rights reserved. No part of this publication may be reproduced without permission.
Running a practice

How to have a great 15-minute therapy consultation

There’s no official guidebook for this important milestone in the therapy journey, but here’s a start for structuring it.

9 therapist referral networks for finding new clients

Here’s how to find and schedule more clients using therapist referral networks and online directories.

When can a therapist break confidentiality, as mandated reporters?

While therapists have an essential responsibility as mandated reporters, it’s challenging to navigate. Learn when a therapist can and must break confidentiality.